A Comprehensive Guide to In Vitro Fertilization (IVF)
In vitro fertilization (IVF) is a sophisticated and multi-faceted medical procedure designed to help individuals and couples achieve pregnancy. As a prominent treatment for infertility, IVF also serves as a solution for preventing genetic disorders from being passed to the next generation. This comprehensive guide explores the ins and outs of IVF, its effectiveness, the preparatory steps, the process itself, and associated risks and considerations.
IVF is a process that involves several key steps aimed at achieving pregnancy. It begins with the stimulation of the ovaries to produce multiple eggs, which are then harvested and fertilized in a laboratory. The resulting embryos are cultured for several days before being transferred into the uterus. This procedure can be an effective solution for various fertility issues that other treatments might not address. In vitro fertilization (IVF) is particularly valuable for those who have struggled with infertility due to conditions such as tubal factor infertility, ovulation disorders, endometriosis, uterine fibroids, male factor infertility, unexplained infertility, or genetic disorders.
IVF can also be a viable option for individuals who wish to preserve their fertility before undergoing treatments that could affect their reproductive capabilities, such as chemotherapy for cancer. Additionally, In vitro fertilization (IVF) provides opportunities for those who need gestational carriers, often referred to as surrogate mothers, to carry the pregnancy when the biological mother cannot.
How IVF Works?
The IVF process involves several critical stages, each playing a crucial role in achieving a successful pregnancy. The cycle typically lasts 2 to 3 weeks, although some aspects of the process might extend this timeframe. Here’s a step-by-step breakdown of how IVF works:
1. Ovarian Stimulation: The first step in In vitro fertilization (IVF) involves stimulating the ovaries to produce multiple eggs. This is achieved through hormonal injections, typically containing follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones encourage the ovaries to develop several eggs instead of the single egg that usually matures each month. During this period, patients undergo regular blood tests and ultrasounds to monitor the development of the follicles, which are fluid-filled sacs in the ovaries that contain the eggs.
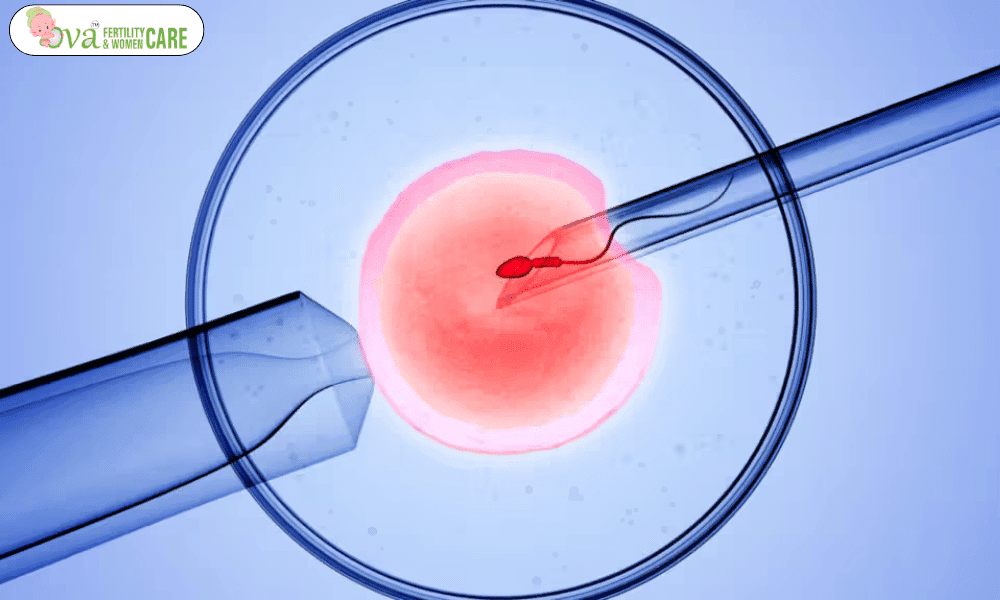
2. Egg Retrieval: Once the eggs are mature, a minor surgical procedure known as egg retrieval is performed. This procedure is usually done under sedation. Using an ultrasound-guided needle, the eggs are aspirated from the ovaries. The process is minimally invasive, but it is essential for the eggs to be collected at the optimal time to ensure their viability for fertilization.
3. Sperm Collection: Sperm collected is carefully processed and prepared to maximize its potential for successful fertilization. In cases where sperm quality or quantity is a concern, techniques such as testicular sperm extraction might be used. The sperm is either mixed with the eggs in a laboratory dish or injected directly into the eggs using a technique called intracytoplasmic sperm injection (ICSI).
4. Fertilization and Embryo Culture: After fertilization, the embryos are monitored as they develop in the lab. This stage typically lasts for about 5 to 6 days. The embryos are assessed for quality and development, with the goal of selecting the most viable embryos for transfer.
5. Embryo Transfer: Once the embryos reach the blastocyst stage, one or more are selected for transfer into the uterus. This procedure involves placing the embryos into the uterus using a thin, flexible tube called a catheter. The transfer is generally straightforward and minimally invasive, though some mild cramping may occur.
6. Post-Transfer Monitoring: After the embryo transfer, patients are monitored for pregnancy. A blood test is conducted approximately 12 days after the transfer to determine if implantation has occurred and if pregnancy has been achieved. If successful, the pregnancy will be monitored through regular obstetric care.

Preparing for IVF?
Preparation for IVF involves several key steps to ensure the best possible outcome. Before starting the IVF cycle, both partners will undergo a series of tests and assessments:
1. Ovarian Reserve Testing: This test assesses the quantity and quality of eggs available in the ovaries. Blood tests measuring hormone levels, along with an ultrasound of the ovaries, provide insights into how the ovaries will respond to stimulation.
2. Semen Analysis: For male partners, a semen analysis evaluates sperm count, motility (movement), and morphology (shape). This test helps identify potential issues with sperm quality and guides the selection of appropriate fertilization techniques.
3. Infectious Disease Screening: Both partners will be screened for infectious diseases such as HIV, hepatitis B, and hepatitis C to ensure the safety of the In vitro fertilization (IVF) process and the health of the baby.
4. Practice Embryo Transfer: This test involves inserting a catheter into the uterus without placing an actual embryo. It helps determine the best technique for the embryo transfer procedure.
5. Uterine Exam: The lining of the uterus is examined to ensure it is suitable for embryo implantation. Tests such as sonohysterography or hysteroscopy may be used to assess the uterine environment.

The IVF Process
The IVF process is intricate and requires careful coordination among medical professionals and patients. Each stage is designed to maximize the chances of successful fertilization and implantation:
1. Ovarian Stimulation and Monitoring: Hormonal medications are administered to stimulate the ovaries. Regular ultrasounds and blood tests are performed to track the development of follicles and ensure that the eggs are maturing properly.
2. Egg Retrieval: The procedure for egg retrieval is performed under sedation. A thin needle is guided through the vaginal wall and into the ovaries to collect the eggs. The process is generally quick, lasting about 20 minutes, and is usually followed by a brief recovery period.
3. Sperm Retrieval and Fertilization: Sperm is collected and prepared for fertilization. The eggs are combined with sperm in a controlled environment. Depending on the quality of sperm and eggs, conventional insemination or ICSI is used to achieve fertilization.
4. Embryo Culture and Transfer: The fertilized eggs develop into embryos over several days. The most viable embryos are selected for transfer into the uterus. The transfer procedure is performed using a catheter, and the embryos are placed in the optimal position for implantation.
5. Post-Transfer Care: Following the embryo transfer, patients are advised to rest and avoid strenuous activities. Symptoms such as mild cramping or bloating may occur, but these are usually temporary.
Risks and Considerations
IVF, while a powerful tool for overcoming infertility, carries certain risks and considerations:
1. Emotional and Financial Stress: The In vitro fertilization (IVF) journey can be emotionally taxing and financially burdensome. Support from counselors, family, and friends is crucial in navigating the ups and downs of the process.
2. Procedural Risks: Complications can arise from procedures such as egg retrieval, including bleeding, infection, or damage to surrounding organs. Ovarian hyperstimulation syndrome (OHSS) is a condition where the ovaries become swollen and painful due to excessive stimulation.
3. Miscarriage and Ectopic Pregnancy: The risk of miscarriage with IVF is similar to that of natural conception but can be influenced by factors such as maternal age. Ectopic pregnancy, where the embryo implants outside the uterus, is also a potential risk.
4. Multiple Pregnancies: IVF increases the likelihood of multiple pregnancies, which can lead to higher risks of pregnancy-related complications such as preeclampsia, gestational diabetes, and premature birth.
5. Birth Defects and Premature Delivery: Some studies suggest a slight increase in the risk of birth defects and premature delivery with In vitro fertilization (IVF). However, the primary risk factor for birth defects remains maternal age.
Conclusion
IVF represents a beacon of hope for many individuals and couples facing infertility challenges. By understanding the detailed process, preparing adequately, and being aware of the potential risks, patients can make informed decisions about their reproductive health. Working closely with a healthcare team ensures that each step is managed effectively, optimizing the chances of a successful pregnancy. In vitro fertilization (IVF) not only offers a path to parenthood for those struggling with infertility but also provides valuable insights and advancements in reproductive medicine.







 No need to worry, your data is 100% Safe with us!
No need to worry, your data is 100% Safe with us!
6 thoughts on “Vitro Fertilization: Step-by-Step IVF Guide | Ova Fertility and Women Care”
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You clearly know what youre talking about, why waste your intelligence on just posting videos to your site when you could be giving us something informative to read?
Admiring the commitment you put into your website and detailed information you present. It’s awesome to come across a blog every once in a while that isn’t the same unwanted rehashed material. Excellent read! I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
Heya! I just wanted to ask if you ever have any trouble with hackers? My last blog (wordpress) was hacked and I ended up losing many months of hard work due to no back up. Do you have any methods to stop hackers?
very nice put up, i actually love this web site, carry on it
Blue Techker Good post! We will be linking to this particularly great post on our site. Keep up the great writing
I like this web site its a master peace ! .